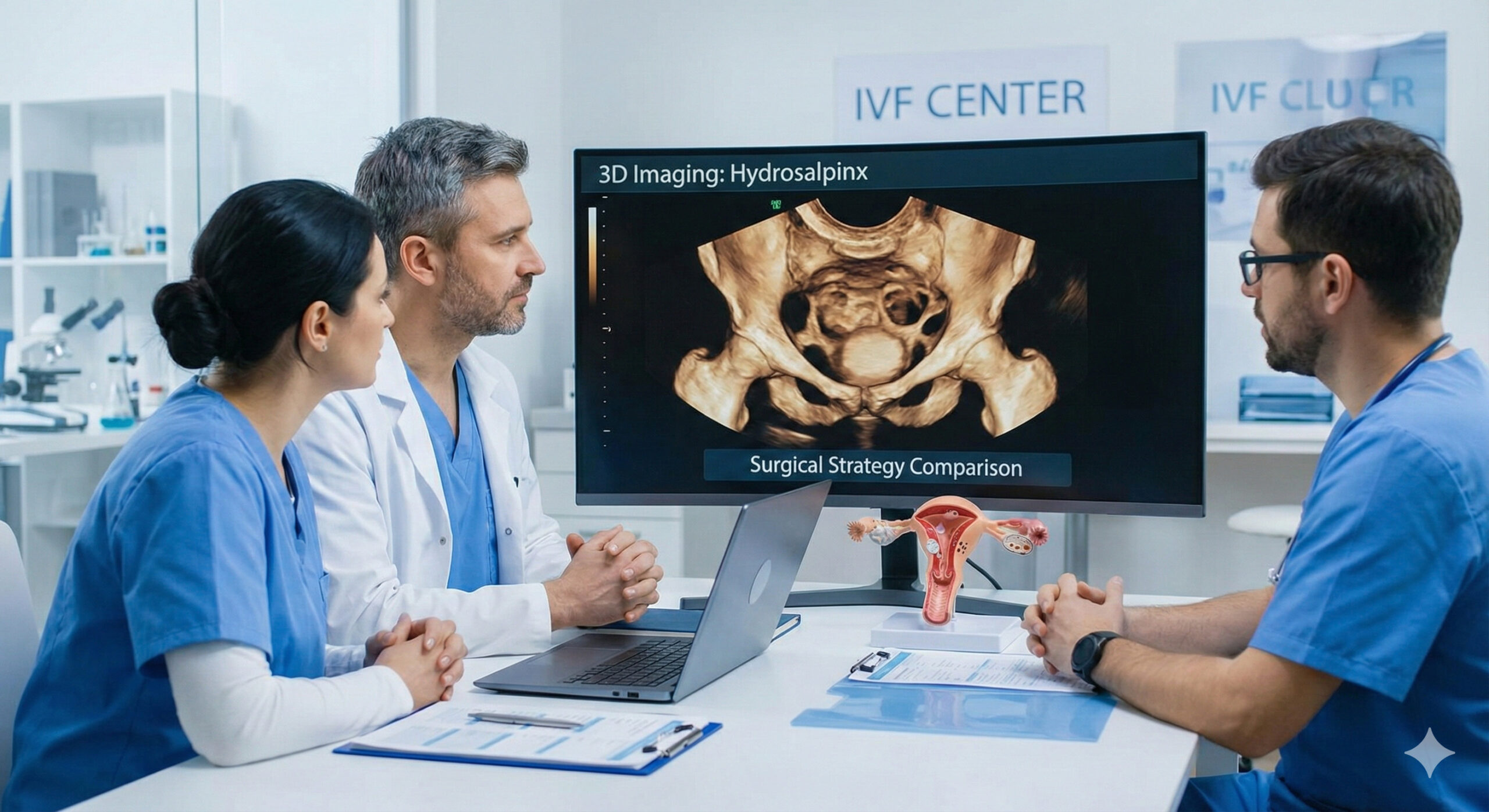
Advanced Clinical Analysis of Hydrosalpinx Management Before In Vitro Fertilization: Comparing Surgical Strategies and the Role of 3D Imaging Diagnostics
Reviewed byDr. Asmita Pandey, MD,Specialist in Obstetrics, Gynecology & ARTI. Executive Summary: The Necessity of Pre-IVF Hydrosalpinx Management The successful outcome of In Vitro Fertilization (IVF) cycles is significantly impaired by the presence of hydrosalpinx (HS), a common pathology among women with tubal-factor infertility.1 Clinical data consistently demonstrate that HS reduces pregnancy, implantation, and ultimately, […]
Recent from Women's Health

Breast health and breast cancer awareness
About the Reviewer Dr. Deepak Shrestha, MD, Associate Professor, Dept. of OBGYN Dr. Deepak Shrestha is a highly experienced Obstetrician and Gynecologist and currently serves as an Associate Professor at Lumbini Medical College. With a career dedicated to maternal health and clinical education, he provides expert oversight on topics ranging from reproductive health to complex […]

Preventive screenings and exams for women, including pap smears and mammograms
About the Reviewer Dr. Deepak Shrestha, MD, Associate Professor, Dept. of OBGYN Dr. Deepak Shrestha is a highly experienced Obstetrician and Gynecologist and currently serves as an Associate Professor at Lumbini Medical College. With a career dedicated to maternal health and clinical education, he provides expert oversight on topics ranging from reproductive health to complex […]

Gynecological health and reproductive issues
About the Reviewer Dr. Deepak Shrestha, MD, Associate Professor, Dept. of OBGYN Dr. Deepak Shrestha is a highly experienced Obstetrician and Gynecologist and currently serves as an Associate Professor at Lumbini Medical College. With a career dedicated to maternal health and clinical education, he provides expert oversight on topics ranging from reproductive health to complex […]

Nutrition and Healthy Eating During Pregnancy and Postpartum: A Guide for Expectant and New Mothers
About the Reviewer Dr. Asmita Pandey, MD Specialist in Obstetrics, Gynecology & Assisted Reproductive Techniques (ART) Dr. Asmita Pandey is a distinguished specialist in Reproductive Medicine, recognized for her clinical expertise and research contributions to the field of fertility. She specializes in Assisted Reproductive Techniques (ART), providing evidence-based solutions for complex reproductive challenges… See Full […]
Sexual health and wellness
Women’s sexual health and wellness are essential for overall health and well- being. Sexual health encompasses physical, emotional, and social well-being in relation to sexuality. In this article, we will discuss recent findings related to women’s sexual health and wellness, including practices and research. Recent Findings Orgasm and sexual satisfaction – A study published in […]

Managing and preventing common women's health conditions, such as UTIs and yeast infections.
Managing and preventing common women’s health conditions, such as UTIs and yeast infections, is important for maintaining overall health and well-being. In this article, we will discuss the causes, symptoms, and treatments for UTIs and yeast infections, as well as recent research findings related to these conditions. Urinary Tract Infections (UTIs) UTIs are a common […]

Maternal health and pregnancy care
Maternal health and pregnancy care are essential for ensuring the health and well- being of both the mother and the baby. In this article, we will discuss the importance of maternal health and pregnancy care, the challenges faced by women during pregnancy, and recent research findings related to this topic. Importance of Maternal Health and […]

Exercise and physical activity for women at different life stages
Exercise and physical activity are essential for women of all ages and stages of life. Regular exercise can help women maintain a healthy weight, reduce the risk of chronic diseases, improve mental health and well-being, and increase overall quality of life. In this article, we will discuss the importance of exercise and physical activity for […]

Mental health and well-being during pregnancy and postpartum
Pregnancy and postpartum can be an exciting and joyful time for many women, but it can also be a challenging and stressful experience. Mental health and well- being during pregnancy and postpartum are critical for the health and well-being of both the mother and the baby. In this article, we will discuss the importance of […]